A 73-year-old female with multiple comorbidities presented to our emergency department in February 2019 after a syncopal episode at dialysis. The patient reported seeing a podiatrist regularly and noted issues with her hammertoe contractions for several years that rubbed on her shoes, leading to sores. Podiatry was consulted to evaluate an infected ulceration on her first left toe.
The patient reported chills and fatigue. Her vital signs included a temperature of 101.8 F, heart rate of 106, blood pressure 155/69 and a respiratory rate of 24. Her pertinent labs included a white blood cell count (WBC) of 7.4, C-reactive protein (CRP) of 0.3 mg/L, an erythrocyte sedimentation rate (ESR) of 60 mm/h, hemoglobin A1C of 6.8%, lactic acid of 1.68 mg/dL and albumin of 3.2 g/dL. The patient had mildly elevated troponin and blood cultures that were positive for Group B Streptococcus beta hemolysis.
The patient noted allergies to cephalexin, ciprofloxacin, codeine, gabapentin, latex, prochlorperazine and divalproex sodium (Depakote, AbbVie). Her past medical history included smoking a pack a day for 30 years prior to quitting in 2010; type 2 diabetes mellitus, peripheral arterial occlusive disease (PAOD), coronary artery disease, end-stage renal disease (ESRD) on dialysis, chronic obstructive pulmonary disease (COPD) on supplemental O2, congestive heart failure (CHF), diastolic heart failure, and epilepsy.
The patient had an extensive list of current medications including apixaban (Eliquis, Bristol-Myers Squibb), clopidogrel, nitroglycerin, fluticasone furoate and vilanterol (Breo Ellipta, GSK), atorvastatin and insulin glargine injection (Lantus Solostar U-100 insulin, Sanofi-Aventis). Her past surgical history included open reduction internal fixation (ORIF) of her right hip, a cardiac stent, fistula placement in 2016 and rotator cuff repair. The social history revealed a patient who was retired, widowed and sedentary. She had a family history of lung cancer and CHF. Her review of symptoms was positive for cramping pain in the back of lower legs, tingling in her feet, chills and fatigue.
During the exam, the patient appeared lethargic and toxic. Her neurovascular status showed severely diminished light touch detection to soles and digits on both feet. Her pedal pulses were non-palpable bilaterally. There were no ischemic changes to the toes on the left foot. The dermatological exam revealed a 0.2 x 0.2 x 0.4 cm ulceration overlying the left hallux interphalangeal joint (IPJ) that probes close to bone with mild surrounding erythema and edema. There was no active purulence from the wound. The patient had atrophy of the intrinsic muscles in both feet. The musculoskeletal exam showed semi-rigid hyperflexion contractions in all toes bilaterally. The ulcer probed close to the head of the proximal phalanx on the first left toe. There was no crepitus with range of motion of the first left toe. Radiographs of the left foot were negative for osteomyelitis of the phalanges of the first left toe. Magnetic resonance imaging (MRI) of the left foot was positive for inflammation within the proximal and distal phalanx, which was concerning for early osteomyelitis.
Arterial doppler studies revealed non-compressible arteries secondary to severe calcification. I was unable to calculate the ankle-brachial index (ABI) tests with this patient so I obtained toe-brachial index (TBI) tests instead that showed 0.27 on the left foot and 0.29 on the right foot.
Wound culture of the first left toe ulcer revealed Group B Streptococcus beta hemolysis, which was the bacterial organism growing in her blood culture. After a subsequent consult with infectious diseases, the patient was placed on meropenem and vancomycin.
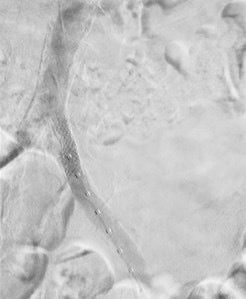
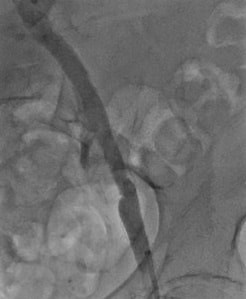
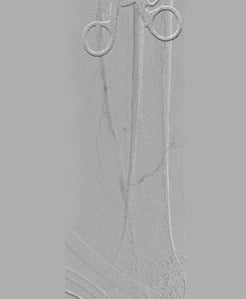
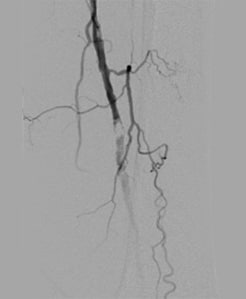
On March 1, 2019, vascular surgeons placed a left common iliac artery stent and performed common femoral and profunda femoris artery endarterectomy with patch angioplasty and a left proximal superficial femoral artery to below-knee popliteal bypass (see Figures 1-4).
I discussed primary partial hallux amputation with the patient but she was adamantly against toe amputation. We discussed the alternative option of hallux arthroplasty with bone culture and biopsy. The patient agreed to proceed with this procedure. The subsequent biopsy was negative for osteomyelitis. Intraoperative culture of the wound revealed Group B Streptococcus beta hemolysis.
The patient was discharged from the hospital with intention of four weeks of IV vancomycin post-discharge and home health care for dressing changes. Her first left toe went on to completely heal three weeks after the surgery and continues to be healed as of her last follow-up visit in April 2021, just over two years since her vascular and podiatry surgeries.
When There Are Setbacks Involving New Ulcerations at Different Locations
The same patient returned in January 2020 with a new complaint of bumping her right leg while at dialysis. She went to the emergency room. While radiographs were negative for fracture, they showed increased swelling on the anterior lateral shin (see Figures 5 and 6). Venous ultrasound was negative for deep vein thrombosis but positive for a complicated pocket suggestive of a hematoma measuring 4.0 x 2.0 x 3.6 cm.
A physical exam of the patient revealed a 10 x 8 x 3 cm raised fluctuant mass overlying the anterolateral right shin. There was surrounding bruising with central epidermal and dermal necrosis. The patient also had non-palpable pedal pulses bilaterally. Treatment consisted of in-office incision and drainage with evacuation of 15 ml of the coagulated hematoma, initiation of oral clindamycin 300 mg every six hours, home health for dressing changes, and subsequent referral to a wound care center.
Upon follow up at the wound care center, clinicians performed a second incision and drainage with evacuation due to the hematoma refilling. Clinicians subsequently packed the wound with iodoform and gave home health instructions on how to change the dressing every other day, ordered updated arterial doppler testing, and scheduled the patient to return for weekly serial wound debridement.
Updated arterial doppler testing revealed triphasic waveforms on the left leg and monophasic waveforms on the right leg with severely diminished toe pressures on the right at 35 mmHg with TBI of 0.21. The left toe pressures were normal with a TBI of 1.03 showing pulsatile flow. Therefore, vascular surgery was reconsulted for concerns of the right leg ulcer.
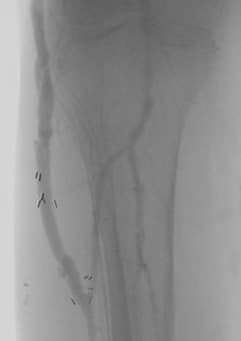
The patient was followed closely for serial wound debridement over the next several weeks (see Figures 7 and 8). She also developed a new ulcer on her fourth right toe secondary to her hammertoe contractions (see Figure 9) and wearing shoes that were too tight. On Feb. 7, 2020, vascular surgery decided to perform an arteriogram with CO2 due to concerns that the patient would not be able to heal her right leg ulcer or toe ulcer spontaneously on her own. Results of the arteriogram showed the previous common iliac artery stent placed on the left side on 3/1/19 was widely patent. On the right side, there was moderate to severe stenosis of the common femoral artery (CFA), a long segment of total occlusion of the superficial femoral artery (SFA), severe stenosis of the popliteal artery (see Figure 10), and moderate stenosis at the origin of the anterior tibial artery.
On 4/20/20, vascular surgery performed external iliac artery and common femoral artery endarterectomy with a pericardial patch angioplasty and a right common femoral artery to anterior tibial artery bypass using composite greater saphenous vein from both legs.
The patient proceeded to rapidly heal her lower right leg ulcer and toe ulcer within three weeks of the vascular intervention (see Figures 11 and 12). She continued to have bouts of superficial ulcers over her contracted digits secondary to ill-fitting shoe gear. Fortunately, subsequent change of her shoe gear to diabetic shoes with tall toe boxes made of a lycra material led to full healing of these toe ulcers. As of April 2021, she continues to have fully healed ulcers and has not had any amputations of her toes.
Updated arterial doppler testing on 9/29/20, a little more than five months after her right leg vascular intervention, revealed biphasic waveforms on the right and triphasic waveforms on the left with pulsatile toe pressures. Bypass graft surveillance testing six months after revascularization of her right leg showed an increase in velocity changes at the mid graft bypass site consistent with moderate stenosis of 50 to 74 percent.
On 2/17/21, updated arterial doppler testing and bypass surveillance was performed for both lower extremities. The patent bypass graft of the lower right leg had no significant velocity changes. The left leg bypass site showed a patent bypass graft with velocity increases suggestive of moderate stenosis.
Due to concerns for restenosis of the distal anastomosis of the left leg bypass along with stenosis of right leg bypass, repeat arteriogram with possible intervention was performed on 3/8/21 (see Figures 13 and 14). No intervention was deemed necessary based on arteriogram findings of only mild stenosis at the bypass sites.
Currently, the patient follows up with podiatry every three to four months for high-risk routine foot care. She remains ulcer-free as of her last visit in April 2021.
Final Notes
This case report is exemplary of the multidisciplinary approach commonly required for limb salvage to be successful. Internal medicine, cardiology, peripheral vascular surgery, infectious disease physicians, social workers, case managers, home health care nurses, nephology, etc, all play a role in helping high-risk patients have a chance at limb salvage. Furthermore, these patients will require lifelong routine follow up with the majority of these providers in order to help avoid any decline in health status.
Vascular interventions, whether they are atherectomies or arterial bypass, have a lifespan of their own and will require routine monitoring to ensure critical restenosis has not occurred.
To treat patients in this high-risk demographic, providers need to be prepared for frequent setbacks. Wound dehiscence, reulceration, transfer ulcers, re-infection and re-occlusion of arterial blockage are the norm, and to be expected. Social barriers, such as transportation or financial constraints leading to no shows to appointments, also lead to poorer outcomes. Therefore, providers will need to be prepared to quickly adjust their clinic schedules to accommodate the needs of these patients.
There is no question that without a multidisciplinary team approach, this patient, along with thousands more with a similar set of comorbidities, would have succumbed to a much poorer outcome.