In an intriguing case involving a patient with a lower extremity burn wound and multiple comorbidities, these authors discuss the multidisciplinary care and targeted revascularization that facilitated healing of a large, complex wound.
A 37-year-old female with a past medical history notable for type 1 diabetes, neuropathy and gastroparesis presented with a third-degree scald burn to her left heel that occurred four days prior to presentation. The patient was showering and did not realize the temperature of the water at the time of the injury due to her severe neuropathy. She initially presented to a different emergency room on the day of the injury. The patient was discharged with topical sulfadiazine for local wound care and outpatient follow-up as the severity and depth of the injury were not immediately identified.
We admitted the patient to our hospital’s burn service, and she had subsequent debridement of her left heel.
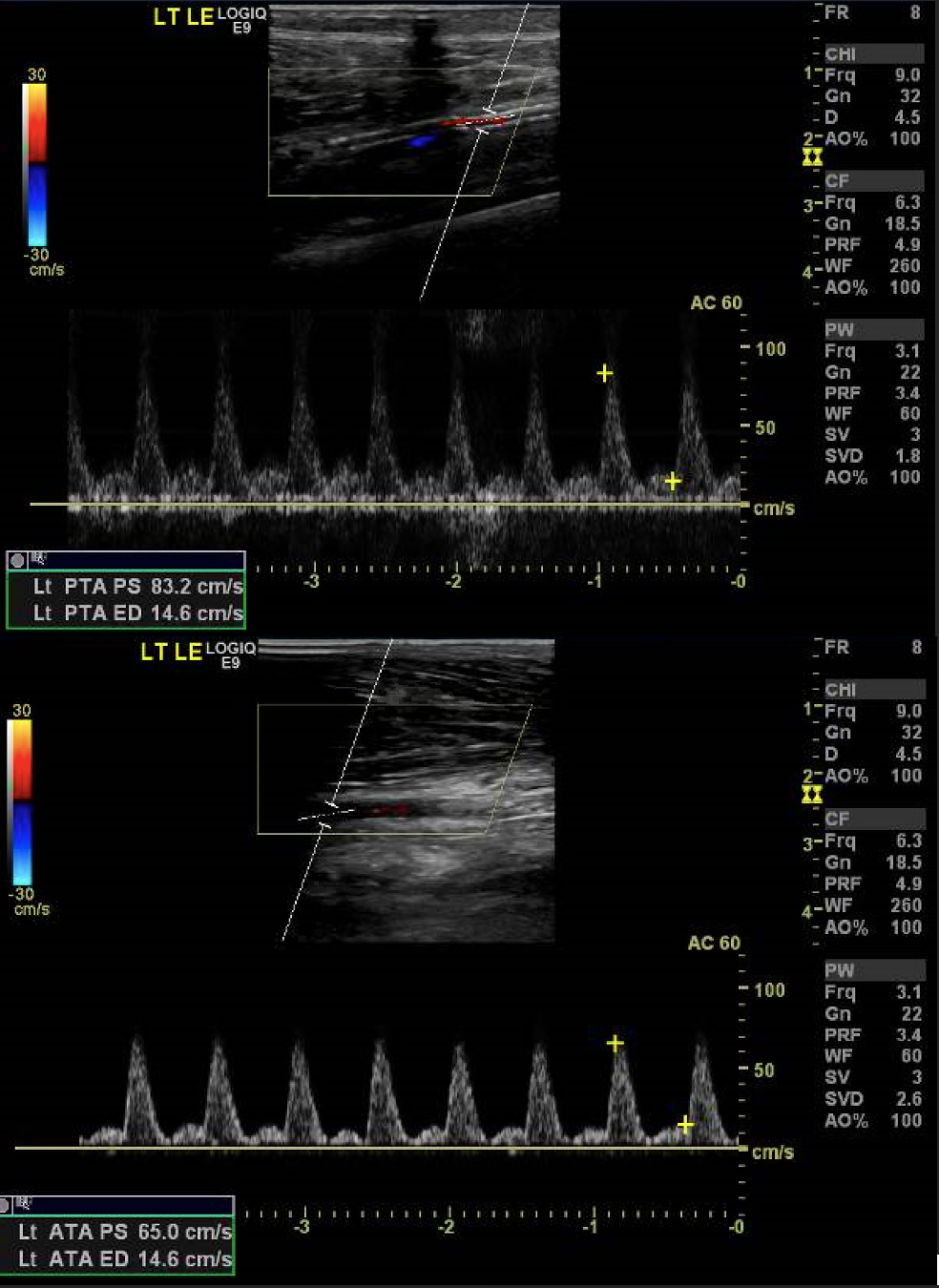
Figure 1
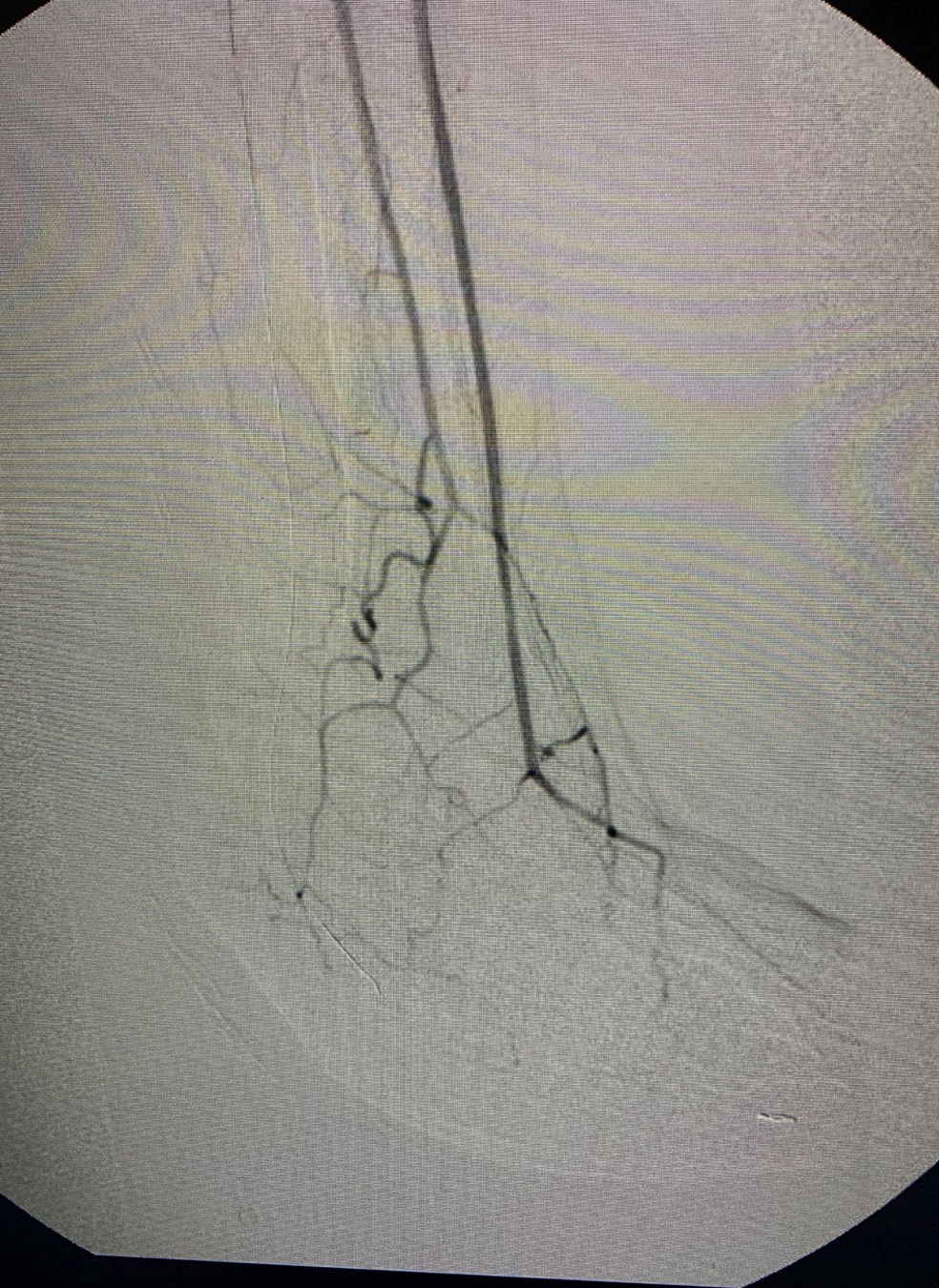
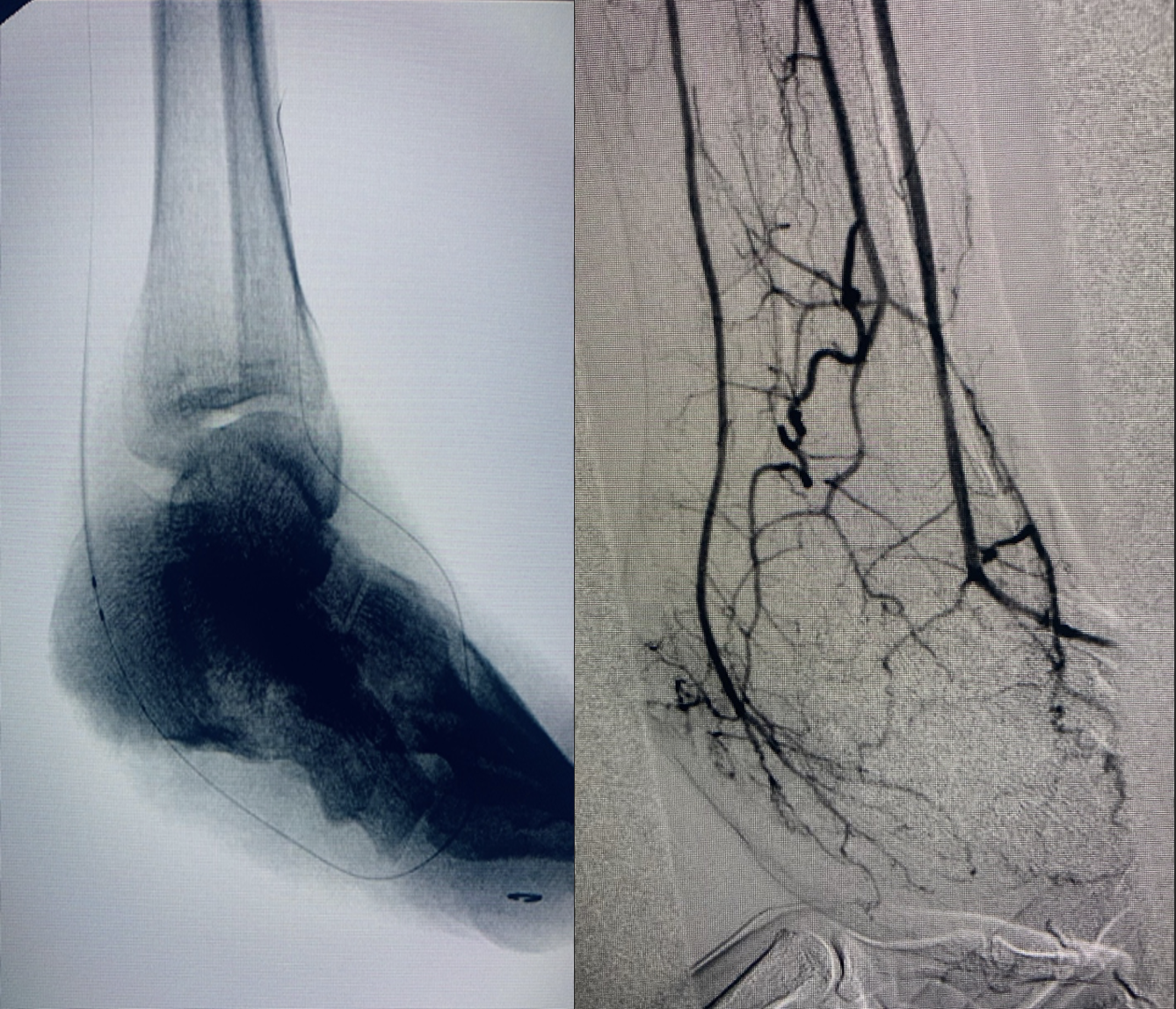
Figure 4
Final Notes
This case serves to elucidate the importance of a multidisciplinary team approach and the angiosome concept. A patient may have inadequate blood flow even in the presence of a palpable distal pulse. Up to 38 percent of ischemic wounds remain unhealed with bypass surgery via indirect revascularization compared to a nine percent failure rate after direct target bypass revascularization.1,2
The angiosome concept, published by Taylor and Palmer in 1987, suggested that specific target vessel revascularization may facilitate improved wound healing and limb salvage over indirect revascularization based on the best available target vessel.1 While this theory was introduced over 30 years ago, it only recently began to gain traction.2,3 Open surgery is less dependent on the angiosome concept and patients appear to respond well with bypass surgery regardless of direct or indirect target revascularization. Bypass surgery is more dependent on adequate collateralization in the foot. With the increasing use of endovascular techniques and a high threshold to perform open surgery, direct target revascularization continues to gain traction as a method for improved outcomes, wound healing, and decreased amputation rates.2,3
Dr. Butler is a second-year resident in General Surgery at the Staten Island University Hospital.
Dr. Culliford is the Director of Plastic, Reconstructive and Hand Surgery at the Staten Island University Hospital.
Dr. Ng is an Assistant Professor at the Donald and Barbara Zucker School of Medicine at Hofstra University and Northwell Health.
Dr. Lopez is an attending podiatrist at the Staten Island University Hospital.
Dr. Singh is the Director of Limb Salvage Surgery and the Vascular Laboratory at the Staten Island University Hospital. He is an Associate Professor at the Donald and Barbara Zucker School of Medicine at Hofstra University and Northwell Health.
References
1. Taylor GI, Palmer JH. The vascular territories (angiosomes) of the body: experimental study and clinical applications. Br J Plast Surg. 1987;40(2):113–41.
2. Lejay A, Georg Y, Tartaglia E, et al. Long-term outcomes of direct and indirect below-the-knee open revascularization based on the angiosome concept in diabetic patients with critical limb ischemia. Ann Vasc Surg. 2014;28(4):983–9.
3. Jongsma H, Bekken JA, Akkersdijk GP, Hoeks SE, Verhagen HJ, Fioole B. Angiosome-directed revascularization in patients with critical limb ischemia. J Vasc Surg. 2017;65(4):1208-1219.e1.