Working in concert with vascular surgeons and infectious disease physicians, these podiatrist authors discuss the diagnostic workup, revascularization, antibiotic management and ultimately successful limb salvage in a patient with peripheral arterial disease and multiple diabetic ulcers in the right foot.
A 64-year-old Caucasian male with type 1 diabetes mellitus and peripheral arterial disease (PAD) presented on August 6, 2020 with diabetic foot ulcers and osteomyelitis (per previous magnetic resonance imaging (MRI)) in the right foot. The patient noted he had been treated with conservative wound care since June 2020. The patient described his foot pain as very sharp and a 10 out of 10 on the visual analog scale (VAS). He reported having chills but denied fever, nausea, vomiting, shortness of breath, or chest pain.
The patient was alert and oriented to time, place and event. He had no known drug allergies. The patient’s prescribed medications included acetaminophen, rosuvastatin, clopidogrel, lisinopril, tramadol, insulin aspart (Novolog, Novo Nordisk) and hydrochlorothiazide. The patient was married. He denied smoking and recreational drug use, and consumed alcoholic beverages two to three times a week. The family medical history was unknown.
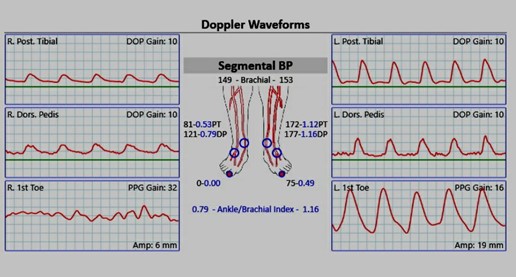
Prior to presentation, the patient had been referred to a vascular surgeon, whom he saw on August 5, 2020. A Doppler ultrasound exam from that evaluation revealed an ankle brachial index (ABI) on the right foot of 0.79 (see Figure 1), but it was deemed inaccurate secondary to calcific sclerosis. The plan was for the patient to have vein mapping in the office and an abdominal arteriogram with runoff to determine vascular options. Unfortunately, the patient was unable to have these procedures done prior to his admission to the hospital.
Figure 1
In addition to the type 1 diabetes mellitus and PAD, the patient’s medical history included hypertension as well as a past cerebrovascular accident (CVA) and intervertebral disc degeneration in 2008. The patient also had a prior appendectomy.
Upon examination, the patient’s vital signs showed an elevated temperature as well as an elevated white blood cell (WBC) count of 14.2 and C-reactive protein (CRP) > 27 mg/L. The dermatologic examination revealed tight, erythematous skin on the plantar right foot extending to the dorsum of the foot; a dusky appearance to the second and fourth toes of the right foot; wounds in the first and fourth interspaces with the 4th interspace wound probing to bone; and malodor without the presence of drainage. Vascular examination revealed a diminished dorsalis pedis pulse on the right foot, diminished capillary refill to all toes on the right foot, and pitting edema to the right foot and anterior leg. Neurologic examination revealed diminished epicritic sensation to the right foot.
Radiographic imaging (see Figure 2) of the right foot showed diffuse soft tissue swelling with intermixed lucencies suggestive of soft tissue gas, and bony destructive changes involving the fourth digit proximal phalanx and likely the adjacent fourth metatarsal head. There were also questionable bony destructive changes of the adjacent fifth digit proximal that were highly suspicious for osteomyelitis.
Figure 2
As per an infectious disease consult, the patient was initially placed on IV vancomycin, cefepime (Maxipime, Hospira), and metronidazole (Flagyl, Pfizer). The vascular surgery team was consulted upon the patient’s hospital admission. He was urgently scheduled for incision and drainage on August 7, 2020 to stabilize the right foot due to the presence of the soft tissue gas. During the surgery, liquefactive necrosis was noted throughout the forefoot, extending from the lateral fourth interspace medially into the first interspace. The fourth metatarsal head was dark and necrotic. We resected this with a sagittal saw and sent it to pathology for culture and review. We also obtained intraoperative samples for aerobic/anaerobic culture and gram stain.
The vascular team performed an arteriogram that same day (August 7, 2021) and it revealed mild-mid superficial femoral artery (SFA) stenosis with 100 percent occlusion of the right proximal anterior tibal (AT) artery with distal reconstitution from peroneal collaterals, 100 percent occlusion of the right distal-posterior tibial (PT) artery with reconstitution from peroneal collaterals, and severe small vessel disease in the dorsalis pedis (DP) and posterior tibial (PT) artery branches. (see Figures 3 and 4).
As per a subsequent infectious disease consult, the patient was switched to piperacillin and tazobactam (Zosyn, Pfizer) due to the growth of many Citrobacter freundii bacteria and few Enterococcus faecalis bacteria and the patient was scheduled for amputation of the first through fifth digits on the right foot. The plan was for the amputation to be packed open and staged. The vascular team performed a below-knee popliteal artery to dorsalis pedis bypass with a reversed right greater saphenous vein, which restored distal flow to the foot.
The patient had the aforementioned surgery on August 11, 2020 with the amputation site packed open. We then performed a transmetatarsal amputation on August 13, 2020, utilized a graft application of Hyalomatrix Hyaluronic Acid Regenerative Matrix (Medline) and allowed for delayed primary closure (see Figures 5 and 6). The patient continued to do well over the next several days and was discharged on August 15, 2020 with PO amoxicillin 1 g BID and sulfamethoxazole/trimethoprim (Bactrim, Sun Pharmaceutical Industries) 1DS BID through August 17, 2020.
Keys To Post-Op Management
We followed up with the patient in clinic weekly for the next month and removed sutures at three weeks. Unfortunately, we noticed on September 16, 2020 that a 2 cm x 2 cm x 0.9 cm fibrogranular wound (which did not probe to bone) at the site of partial closure had increased in size along with increased periwound erythema. Due to the increasing signs of infection, the patient was told to go to the hospital for pre-admission in order to receive IV antibiotics and further surgical intervention.
The patient was initially placed on IV vancomycin and cefepime per an infectious disease consult. He was taken back to the OR on September 18, 2020 for a formal debridement of the wound with subsequent graft application of Hyalomatrix and use of negative pressure wound therapy (VAC therapy, KCI/3M). The patient was eventually cleared for hospital discharge on September 21, 2020 and sent home with prescriptions for PO cefuroxime 500 mg and metronidazole 500 mg TID. The plan was for the patient to continue using VAC therapy with serial dressing changes three times per week and to follow up every two weeks as an outpatient in the clinic.
The first follow-up visit with the patient was on October 23, 2020. At this time, the debrided wound was 1.5 x 1.5 cm, and appeared to be granular and healthy. The patient was instructed to remain non-weightbearing with the right foot until there was further healing of the graft site and wound. He was placed in a surgical shoe to help protect the foot and was given instructions for every other day dressing changes with Promogran Prisma Wound Balancing Matrix (KCI/3M) and dry sterile dressings. Over the next several weeks, the wound began to further epithelialize and was gently debrided at each visit with a 15 blade. The patient continued to use the collagen dressings and he eventually transitioned to wearing a diabetic shoe with carbon plate insert. At the last follow-up visit on June 4, 2021, the wound was completely healed with slight skin fissuring noted laterally.
In Conclusion
This case study revealed that a multispecialty approach to limb salvage is critical to patient success. The podiatry team worked closely with the vascular team to ensure appropriate timing of surgical intervention to facilitate optimal treatment outcomes for the patient’s right foot. This case study also emphasizes the importance of the staged approach to diabetic limb salvage. However, despite a multispecialty and staged approach to limb salvage, complications can occur. In the case of this patient, the use of graft applications (to help with reepithelialization) and VAC therapy were beneficial in overcoming the complications we encountered.
Dr. Alvarez is a second-year resident at the Ascension St. Vincent Hospital in Indianapolis.
Dr. Patel is a fourth-year student at the Dr. William M. Scholl College of Podiatric Medicine at the Rosalind Franklin University of Medicine and Science.
Dr. Wolfe is an attending physician at the Ascension St. Vincent Hospital in Indianapolis.