The American Limb Preservation Society is dedicated to ending preventable amputations through innovative approaches and multidisciplinary collaboration. We want to showcase the impact limb preservation teams can have on patient outcomes. This article highlights the vascular-podiatric surgery foot program at Broomfield Hospital, a shining example of how collaborative efforts can significantly reduce major foot amputations.

The Mid Essex Diabetes Amputation Reduction Plan (MEDARP) at Broomfield Hospital aimed to improve the treatment of patients with diabetic foot ulceration to meet The National Institute of Health and Care Excellence (NICE) standards. The service model was inspired by the Manchester Amputation Reduction Strategy (MARS), which successfully implemented the toe and flow model. The Broomfield program brought together a dedicated team, including a full-time podiatrist and a part-time consultant podiatric surgeon, who worked alongside vascular, plastics and other members of the multi-disciplinary diabetic foot team who were already established departments to optimize care.
Key Success Factors
The creation of the vascular-podiatric surgery foot program at Broomfield Hospital was driven by the presence of key clinicians within the system who were not yet working in a coordinated manner. Integrating podiatric surgery helped reduce waiting times for patients requiring limb preservation surgery. This initiative was funded by external diabetes funding from the government, which allowed the natural progression into a toe and flow model of care. Despite time and limited funding, the program’s success was evidenced with local system support.
Addressing Challenges
Implementing the program faced challenges, particularly the lack of dedicated administrative support, which placed additional burdens on clinicians. The vascular and diabetes teams, however, dedicated their time to support the program, ensuring its sustainability. Michelle Goodeve, project manager and lead podiatrist, emphasizes, “Working together in teams reduces duplication of appointments, speeds up surgical care plans, decreases hospital stays, and saves money. It is crucial for healthcare professionals to prioritize multidisciplinary approaches to improve patient outcomes.”

Ewan Kannegieter (Consultant Podiatric Surgeon), Michelle Goodeve (Podiatrist and MEDARP Project Lead) and Fiona Maguire (Vascular Nurse)
Impact and Outcomes
Over the pilot’s three-year timeframe, the program recorded over 1,000 ward and outpatient department (OPD) patient contacts and 84 day-case wide-awake surgical admissions, totaling 316 procedures aimed at preserving limb and life. The program provided expertise in ulcer management and limb preservation surgery across various hospital departments.
Ewan Kannegieter, a key contributor to the program, noted, “Outcomes from surgery have been extensively audited with validated patient reported outcome measures (PROMs), with 94.7% stating they would have surgery again in the same circumstances. PROMs demonstrate improvement across multiple patient domains including walking/standing, social interaction, pain levels, and most importantly self-reported physical activity increased post-surgery rising from 1.6 days out of 7, to 4.2 at a mean of 11 months.”
Economic analyses, such as those by Kerr (2017), reveal the high cost of diabetic foot ulcers, averaging £359 per week. Before referral to the pilot OPD clinic, patients spent an average of 87 weeks in community settings for ulcer care, costing the local healthcare system an estimated £2,623,572; the cost of not seeing a MDFT earlier for the 84 surgical cases alone. The program has significantly reduced these costs by ensuring patients are seen within one week of referral and, if necessary, receive surgical intervention within four weeks.
Patient Success Story: Limb Preservation at Broomfield Hospital
Case Overview:
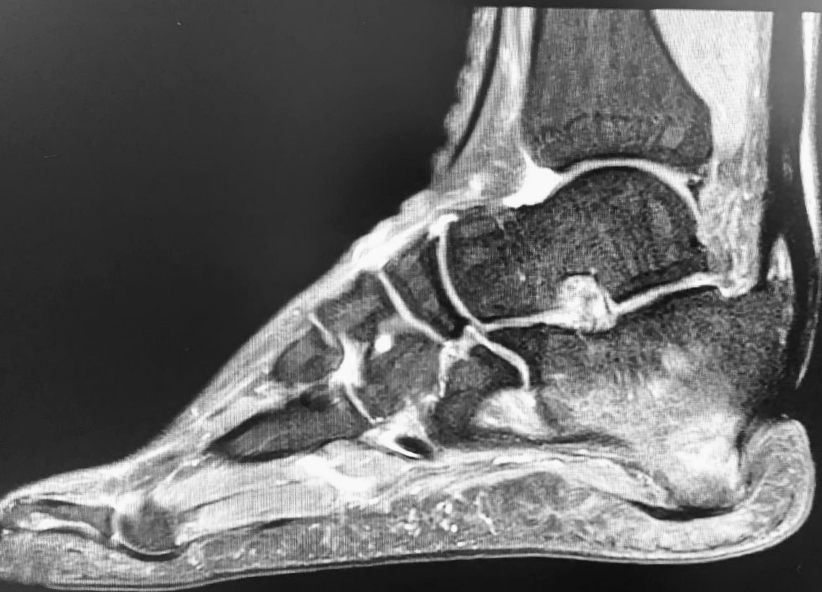
A patient with a 10-year history of calcaneal osteomyelitis, suffering from posterior heel tissue loss and significant bone changes, sought care at Broomfield Hospital. Without previous multidisciplinary team (MDT) intervention, the patient’s condition had deteriorated.
Innovative Treatment:
Under the comprehensive care model of Broomfield’s vascular-podiatric surgery program, the patient underwent a joint podiatric and plastics surgery admission. The procedure included debridement, calcaneal reshaping, and the application of Cerament antibiotic cement. A free flap was used to cover the deficit, all performed in one hospital admission and one trip to the operating theatre.
Remarkable Outcomes:
The patient’s recovery was closely monitored:
- 6 weeks post-op: Initial healing progress evident.
- 6 months post-op: Continued improvement with no signs of infection.
- 1 year post-op: Full recovery, with no recurrence of ulceration or need for wound care.
Current Status:
Three years post-surgery, the patient remains free of ulceration and infection, exemplifying the success of Broomfield’s multidisciplinary approach in limb preservation.
The Importance of Multidisciplinary Teams
The success of Broomfield’s program underscores the importance of multidisciplinary teams working with a toe and flow model. Michelle Goodeve highlights several key benefits of this approach. With the increasing prevalence of diabetes and a declining specialist workforce, working in teams maximizes the use of available expertise and reduces redundant appointments, thus speeding up care plans. This approach also decreases hospital stays and alleviates pressures on inpatient services, leading to significant cost savings and compliance with NICE and IWGDF guidelines. Most importantly, it improves patient-reported outcomes (PROMs) and quality of life, demonstrating substantial improvements in walking/standing, social interaction, pain levels, and self-reported physical activity.
Looking Ahead
The vascular-podiatric surgery foot program at Broomfield Hospital exemplifies the transformative power of multidisciplinary approaches in limb preservation. “At the American Limb Preservation Society, we recognize the critical role that Broomfield Hospital’s Vascular-Podiatric Surgery Program plays in advancing limb preservation. The success of such programs lies in their commitment to a multidisciplinary approach, bringing together experts from various fields to provide comprehensive care. This collaboration is essential for optimizing patient outcomes and preventing amputations, ultimately improving the quality of life for those at risk,” said Georgia Krehbiel, ALPS CEO. ALPS encourages healthcare professionals to consider forming similar teams to improve patient outcomes and advance limb preservation efforts globally. By joining ALPS, professionals can network, share knowledge, and collaborate to drive innovation in this critical field.
For more information about the vascular-podiatric surgery foot program at Broomfield Hospital, please contact Ewan Kannegieter at ewan.kannegieter1@nhs.net.
For more information on how to form your own limb preservation team and the benefits of ALPS membership, please visit our website.