Dr. Meghan Brennan, infectious disease physician, implementation scientist, and the 2024 ALPS Traveling Fellow, shares reflections on a fellowship experience that spanned the University of Michigan and Oxford. She discusses learning what she didn’t know she needed to know, the value of co-designing a clinical visit, and why this welcoming community made her feel right at home, even when cold-emailing world experts.
“[…]I learned that this is a very, very welcoming community. Yes, you’re going to feel awkward sending those emails. But the person receiving them will- nine times out of ten- be excited to host.” – Dr. Meghan Brennan
ALPS: Tell us a little about your background. What led you into infectious disease and eventually diabetic foot care?
Dr. Brennan: From a very, very early age I knew I wanted to be an infectious disease doc. You could have asked me in grammar school, and I would have said, “Yes, that’s what I’m going to do.”
As for specializing in diabetic foot ulcers, honestly, it started because there was a clear need. My division chief suggested it as an area that was ripe for research because it wasn’t being studied in a standardized fashion. So, I started hanging out with podiatrists, and it turns out I really like them. They have very minimal egos, and that’s something that especially appeals to me. They’re just there to serve the patient and do the right thing.
ALPS: What was most outstanding about your fellowship experiences in Michigan and Oxford?
Dr. Brennan: I would, 100%, wake up and do it all over again.
For me, the best thing about the fellowship was that I could make it whatever I wanted. My institute is in the middle of setting up a multidisciplinary clinic, so I wanted to learn how other people started successful diabetic foot ulcer teams. I was really focused on how they incorporated research and how they triaged patients. What I found was that it’s actually easy to incorporate research once you have your team up and running. If that’s going smoothly, everything else seems to fall into place.
ALPS: Was there anything that surprised you during the visits?
Dr. Brennan: Yes, definitely. For both sites, there were things that fell into the category of “you don’t know what you don’t know.” And I think one of the smartest things we did was iron out an itinerary that had two parts: stuff I knew I wanted to learn, and things the host knew were outstanding even if I didn’t ask about them.
In Michigan, for example, I learned about their incredible lymphedema clinics and how much everyone works to the top of their license. In Oxford, I wouldn’t even have known to ask about their triage system, because it’s so different from what we do here in the U.S. But once I saw it, I couldn’t stop thinking about how valuable that structure is.
ALPS: What did you take away about turning that knowledge into action back home?
Dr. Brennan: Systems are different, so of course you’re not going to come home and just copy-paste something. You can’t say, “Let’s do that exact thing here.” But there are still a lot of actionable pieces. You come away from the fellowship knowing those nuggets, and you’re primed to feed that knowledge back to your institution and your colleagues when you return.
When I came back from both sites, I had meetings with the folks who were helping form our multidisciplinary clinic. They were basically structured as debriefs, and they made a big difference. Once you know what you want to do, even if it’s a heavy lift, it becomes easier because you’re lifting it with your peers and using those tools your predecessors built.
ALPS: What stage are you in now with your multidisciplinary team?
Dr. Brennan: When I started the ALPS Fellowship, we were still presenting proposals for a multidisciplinary clinic to our administration. When I went to Michigan, we we were about 90% through the administration hoops. By the time I got to Oxford, we had secured nursing FTEs and space.
We’re set to launch in early 2026. So the timing of the fellowship was absolutely ideal. I could compare what I saw with what we were building and can implement ideas I learned.
ALPS: Did you find that you had to convince others of the value of an MDT, or was that support already there?
Dr. Brennan: I didn’t have to convince anyone, which is great. For clinicians, it’s just so obvious that working together is the right thing to do. Once you have that shared vision, it’s just about logistics—how to staff it, how to structure it, how to make it sustainable.
ALPS: What advice would you give to someone considering applying for the ALPS Traveling Fellowship?
Dr. Brennan: If you’re on the fence, apply.
“Cold calling” the places you want to go to get a letter of support and see if they would be willing to host was nerve-wracking for me. But I learned that this is a very, very welcoming community. Yes, you’re going to feel awkward sending those emails. But the person receiving them will- nine times out of ten- be excited to host.
I also think one of the smartest things I did was co-designing my itinerary. You know what you want to learn, but the host knows what’s great about their site. You want both perspectives going in. That’s how you get the most out of it.
ALPS: If you were to describe the whole experience of the ALPS Traveling Fellowship in three words or less, what would they be?
Dr. Brennan: Totally underrated.
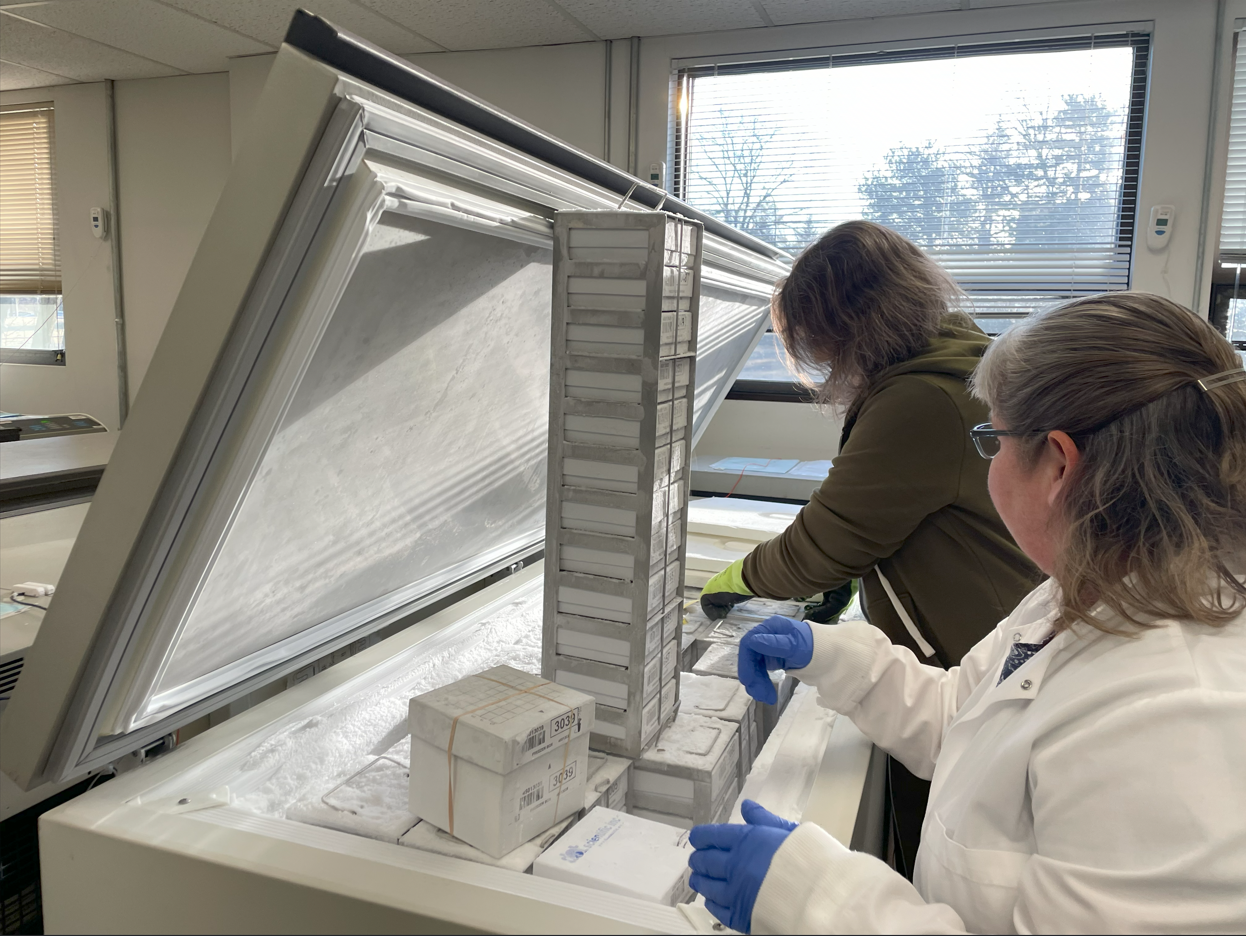
A photo of the Diabetic Foot Consortium’s central storage facility (and freezer boxes of safely housed clinical specimens). All specimens are stored at the Coordinating Center at the University of Michigan
About the ALPS Traveling Fellowship:
The ALPS Traveling Fellowship is a unique initiative that supports early- to mid-career healthcare professionals in expanding their expertise within the field of limb preservation. With up to $7,500 in funding, fellows are given the opportunity to visit two international centers of excellence, each for one week, to observe, learn, and collaborate across specialties. The goal is to strengthen interdisciplinary, team-based approaches to patient care—an essential part of ALPS’s mission to eliminate preventable amputations.
Fellows are encouraged to select host institutions that not only align with their own field (such as vascular surgery, podiatry, infectious disease, or rehabilitation), but also expose them to complementary disciplines. While the fellowship is not designed to fund research projects, it frequently opens the door to impactful academic and clinical collaborations.
Applicants must be active members of ALPS in order to apply.
To see what this journey looks like in practice, read about the experience of Dr. Michael Siah, the 2023 ALPS Traveling Fellow, who visited world-renowned limb salvage expert Dr. Roberto Ferraresi in Milan, Italy:
Bridging Borders, Saving Limbs: Dr. Michael Siah’s Journey with the ALPS Traveling Fellowship
For full details on how to apply, visit the official ALPS Traveling Fellowship page here:
https://limbpreservationsociety.org/traveling-fellowship